What 3 Arteries Leave the Aorta and Where Do They Suply Blood to
Some changes in the heart and blood vessels normally occur with age. However, many other changes that are common with aging are due to or worsened by modifiable factors. If not treated, these can lead to heart disease.
BACKGROUND
The heart has two sides. The right side pumps blood to the lungs to receive oxygen and get rid of carbon dioxide. The left side pumps oxygen-rich blood to the body.
Blood flows out of the heart, first through the aorta, then through arteries, which branch out and get smaller and smaller as they go into the tissues. In the tissues, they become tiny capillaries.
Capillaries are where the blood gives up oxygen and nutrients to the tissues, and receives carbon dioxide and wastes back from the tissues. Then, the vessels begin to collect together into larger and larger veins, which return blood to the heart.
AGING CHANGES
Heart:
- The heart has a natural pacemaker system that controls the heartbeat. Some of the pathways of this system may develop fibrous tissue and fat deposits. The natural pacemaker (the sinoatrial or SA node) loses some of its cells. These changes may result in a slightly slower heart rate.
- A slight increase in the size of the heart, especially the left ventricle occurs in some people. The heart wall thickens, so the amount of blood that the chamber can hold may actually decrease despite the increased overall heart size. The heart may fill more slowly.
- Heart changes often cause the electrocardiogram (ECG) of a normal, healthy older person to be slightly different than the ECG of a healthy younger adult. Abnormal rhythms (arrhythmias), such as atrial fibrillation, are more common in older people. They may be caused by several types of heart disease.
- Normal changes in the heart include deposits of the "aging pigment," lipofuscin. The heart muscle cells degenerate slightly. The valves inside the heart, which control the direction of blood flow, thicken and become stiffer. A heart murmur caused by valve stiffness is fairly common in older people.
Blood vessels:
- Receptors called baroreceptors monitor the blood pressure and make changes to help maintain a fairly constant blood pressure when a person changes positions or is doing other activities. The baroreceptors become less sensitive with aging. This may explain why many older people have orthostatic hypotension, a condition in which the blood pressure falls when a person goes from lying or sitting to standing. This causes dizziness because there is less blood flow to the brain.
- The capillary walls thicken slightly. This may cause a slightly slower rate of exchange of nutrients and wastes.
- The main artery from the heart (aorta) becomes thicker, stiffer, and less flexible. This is probably related to changes in the connective tissue of the blood vessel wall. This makes the blood pressure higher and makes the heart work harder, which may lead to thickening of the heart muscle (hypertrophy). The other arteries also thicken and stiffen. In general, most older people have a moderate increase in blood pressure.
Blood:
- The blood itself changes slightly with age. Normal aging causes a reduction in total body water. As part of this, there is less fluid in the bloodstream, so blood volume decreases.
- The speed with which red blood cells are produced in response to stress or illness is reduced. This creates a slower response to blood loss and anemia.
- Most of the white blood cells stay at the same levels, although certain white blood cells important to immunity (neutrophils) decrease in their number and ability to fight off bacteria. This reduces the ability to resist infection.
EFFECT OF CHANGES
Normally, the heart continues to pump enough blood to supply all parts of the body. However, an older heart may not be able to pump blood as well when you make it work harder.
Some of the things that make your heart work harder are:
- Certain medicines
- Emotional stress
- Physical exertion
- Illness
- Infections
- Injuries
COMMON PROBLEMS
- Angina (chest pain caused by temporarily reduced blood flow to the heart muscle), shortness of breath with exertion, and heart attack can result from coronary artery disease.
- Abnormal heart rhythms (arrhythmias) of various types can occur.
- Anemia may occur, possibly related to malnutrition, chronic infections, blood loss from the gastrointestinal tract, or as a complication of other diseases or medicines.
- Arteriosclerosis (hardening of the arteries) is very common. Fatty plaque deposits inside the blood vessels cause them to narrow and totally block blood vessels.
- Congestive heart failure is also very common in older people. In people older than 75, congestive heart failure occurs 10 times more often than in younger adults.
- Coronary artery disease is fairly common. It is often a result of atherosclerosis.
- High blood pressure and orthostatic hypotension are more common with older age. Older people on blood pressure medicines need to work with their doctor to find the best way to manage their high blood pressure. This is because too much medicine may cause low blood pressure and could lead to a fall.
- Heart valve diseases are fairly common. Aortic stenosis, or narrowing of the aortic valve, is the most common valve disease in older adults.
- Transient ischemic attacks (TIA) or strokes can occur if blood flow to the brain is disrupted.
Other problems with the heart and blood vessels include the following:
- Blood clots
- Deep vein thrombosis
- Thrombophlebitis
- Peripheral vascular disease, resulting in intermittent pain in the legs when walking (claudication)
- Varicose veins
- Aneurysms may develop in one of the major arteries from the heart or in the brain. Aneurysms are an abnormal widening or ballooning of a part of an artery due to weakness in the wall of the blood vessel. If an aneurysm bursts it may cause bleeding and death.
PREVENTION
- You can help your circulatory system (heart and blood vessels). Heart disease risk factors that you have some control over include high blood pressure, cholesterol levels, diabetes, obesity, and smoking.
- Eat a heart-healthy diet with reduced amounts of saturated fat and cholesterol, and control your weight. Follow your health care provider's recommendations for treating high blood pressure, high cholesterol or diabetes. Reduce or stop smoking.
- Men between the ages of 65 to 75 who have ever smoked should be screened for aneurysms in their abdominal aorta usually with an ultrasound exam.
Get more exercise:
- Exercise may help prevent obesity, and it helps people with diabetes control their blood sugar.
- Exercise may help you maintain your abilities as much as possible, and it reduces stress.
- Moderate exercise is one of the best things you can do to keep your heart, and the rest of your body, healthy. Consult with your provider before beginning a new exercise program. Exercise moderately and within your capabilities, but do it regularly.
- People who exercise often have less body fat and smoke less than people who do not exercise. They also tend to have fewer blood pressure problems and less heart disease.
Have regular check-ups for your heart:
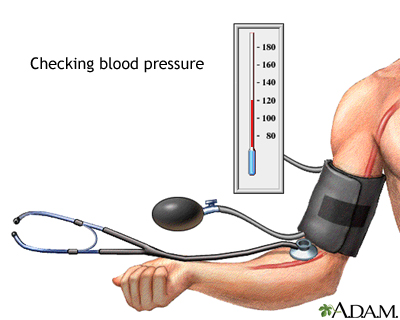
- Have your blood pressure checked every year. If you have diabetes, heart disease, kidney problems, or certain other conditions, your blood pressure may need to be monitored more closely.
- If your cholesterol level is normal, have it rechecked every 5 years. If you have diabetes, heart disease, kidney problems, or certain other conditions, your cholesterol may need to be monitored more closely.
Heart disease - aging; Atherosclerosis - aging
Forman DE, Fleg JL, Wenger NK. Cardiovascular disease in the elderly. In: Zipes DP, Libby P, Bonow RO, Mann DL, Tomaselli GF, Braunwald E, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 11th ed. Philadelphia, PA: Elsevier; 2019:chap 88.
Howlett SE. Effects of aging on the cardiovascular system. In: Fillit HM, Rockwood K, Young J, eds. Brocklehurst's Textbook of Geriatric Medicine and Gerontology. 8th ed. Philadelphia, PA: Elsevier, 2017:chap 16.
Seki A, Fishbein MC. Age-related cardiovascular changes and diseases. In: Buja LM, Butany J, eds. Cardiovascular Pathology. 4th ed. Philadelphia, PA: Elsevier Saunders; 2016:chap 2.
Walston JD. Common clinical sequelae of aging. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 26th ed. Philadelphia, PA: Elsevier; 2020:chap 22.
Updated by: David C. Dugdale, III, MD, Professor of Medicine, Division of General Medicine, Department of Medicine, University of Washington School of Medicine. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
What 3 Arteries Leave the Aorta and Where Do They Suply Blood to
Source: https://medlineplus.gov/ency/article/004006.htm
0 Response to "What 3 Arteries Leave the Aorta and Where Do They Suply Blood to"
Post a Comment